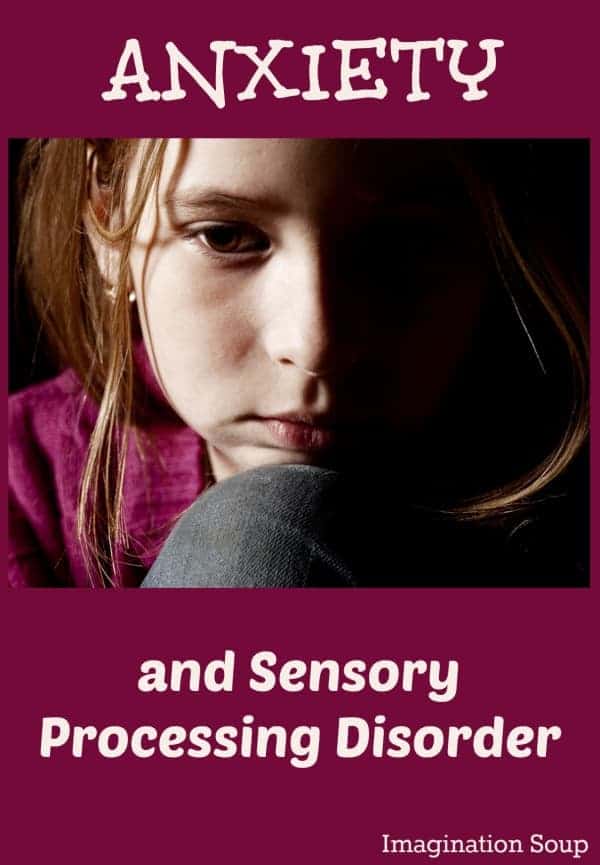
Our Daughter’s Anxiety Connected to Sensory Processing Disorder
This post may contain affiliate links.
A few years ago we wondered if AJ had sensory processing disorder, SPD, and if it related to her anxiety.
Sensory Processing Disorder
At the time, her anxiety was so overwhelming, she had trouble leaving the house. She’d curl up in the fetal position and cry. A lot. (It sucked.)
Anxiety, if you ever have experienced it, doesn’t make sense.
After a miserable mountain vacation trapped in our condo, I realized that she needed more help than I could give. Professional help.
So, we went to a therapist. Well, two cognitive therapists. (In retrospect, I would recommend finding a good art or play therapist. That’s another blog post though.)
After seven months or so of weekly therapy sessions and little improvement, the last therapist suggested we get AJ evaluated at Children’s Hospital for SPD.
Fast forward to a diagnosis — SPD with tactile over-responsiveness. In other words, her tactile sensory system was over stimulated all the time. It explained everything – like why she hated to be held as a baby, why she flinched when we hugged her, or why the lining of her socks had to be smooth and thread free. Maybe, it explained the anxiety. We would soon find out.
Occupational Therapy at Children’s
We started occupational therapy at Children’s. Sabrina, the wonderfully kind OT, gave us weekly homework including a brushing technique and joint compressions.
Brushing and compressions worked miracles – which is bizarre because they seemed a bit like voodoo. But the proof was the result . . . after only a few months, she was a different kid.
The biggest immediate result? The anxiety disappeared. (And with it, the curled-up in a fetal position melt-downs.)
Another reward of the therapy? Hugs and the occasional cuddle. Soon, AJ wanted me to lay down with her while she fell asleep. We had some catching up to do! I got to make up for so many years where she didn’t want to be touched.
Update
We didn’t do the therapy forever – at home or at Children’s. For one, it was just too expensive. We stopped when we saw results after about 9 months.
Now, when we see that AJ’s over stimulated or seems “off,” we’ll start brushing again for a few days. Sometimes we give her a full-body, super tight-squeeze bear hug. It immediately calms her down. (I know, it seems weird for a touch-sensitive person but totally works!)
AJ is growing into herself every day, without the interference of her over-stimulated senses. She’s an amazing child with a lot to offer the world. If it weren’t for us discovering SPD, we wouldn’t be where we are today.
 Which is why I’m telling you this. Only very recently are doctors considering SPD a legitimate diagnosis. But whether or not it’s in the DSM or people think it’s a “fad,” it’s a very real condition. And something you get help for.
Which is why I’m telling you this. Only very recently are doctors considering SPD a legitimate diagnosis. But whether or not it’s in the DSM or people think it’s a “fad,” it’s a very real condition. And something you get help for.
Further Reading
Sensory Processing Disorder involves one or more of the senses and can be either over-responsive or under-responsive. The opposite of AJ is tactile under-responsive, also called a sensory seeker. These are kids who always are touching you, in your lap, petting others, hugging, seeking to be touched. I know of kids whose affected senses are hearing and vision.
SPD Foundation’s website
“Is it Sensory Processing or ADHD?”, ADDitude Magazine
SPD Blogger Network
I hope this helps you – or someone you know.
Do you have any questions for me? Experiences with this?
UPDATE: How Developing the Brain Helped with Sensory Processing, Anxiety & Food Pickiness For Our Kids
My first post about SPD . . .


We’ve been successfully working through our daughter’s anxiety for just over 6 years. We depend on Lemon Balm and keeping her busy. Competitive gymnastics has been amazing. But, at a mock meet when there was much less going on, lots of quiet, and only 2 events, she turned into rubber and broke her arm. It may be time for us to take the next step. I would really love to hear more of AJ’s behaviors and corresponding ages that were displayed due to spd/anxiety. We’re dealing with anger and occasional violence. Yup. Thanks
Up until the time we did the therapy recommended by the OT at children’s (brushing, etc) she had meltdown tantrums — I suspect these would have continued until we did the therapies no matter what her age.
She is not “cured” but so able to handle life so much better. When she has flare ups with behavior, I do the brushing again with her (she hates it and fights it- oh, joy) and that helps — also big bear hugs help calm her down.
My pediatric psychologist college, Dr. Lynne Kenney, reminded me that she feels like her skin is on inside out — and to continue having compassion for her instead of my first reaction of just weary annoyance / anger. That helped. My husband has to remind me of that A LOT when I get triggered by certain behaviors.
I think it’s this parenting thing is hardest thing I’ve ever done!
Does that help? Have you tried OT / brushing?
I just came across your wonderful article about your daughter! I look forward to reading the rest of the page, with everyone’s comments.
Let me know what you think about my experience on my site.
Thank you a lot for giving everyone remarkably breathtaking possibility to read from this web site.
It is often very fantastic plus jam-packed with amusement for
me personally and my office acquaintances to visit the blog at least thrice weekly to find out the latest stuff you will have.
And definitely, I’m just actually satisfied with all the impressive creative
concepts you give. Selected 3 points on this page are easily the simplest I’ve ever had.
Thanks for sharing your story with everyone. We are currently going to OT for sensory processing for my 3yo son. He hasn’t started school yet, but will be going to pre-school next week. Is there anything they (teachers) can do in the classroom to help? Will they recognize it as a real problem when I explain it to them?
Here are some ideas — https://imaginationsoup.net/2015/09/classroom-strategies-for-sensory-processing-disorder/ — I think some teachers are knowledgable about SPD while others aren’t. It just depends on the teacher and administration. Best wishes for a good school year!
Oh boy…our journey with SPD began about two years ago. It took another year to diagnose. Our challenge was not only to find a therapist who could help but to also find someone who would not go straight to medication. At the time, she was 6 and I could not justify putting her on medication as a first resort. Since then, we have worked with therapists, including OTs, to get some semblance of control over it. The brushing you mentioned with your daughter is a very effective technique with us too, as are joint compression. We are also having significant luck by monitoring the food she eats: trying to eat non-processed foods, staying away from food dyes (huge triggers). We still have meltdowns. In fact, just had a a major one this morning, but the frequency has diminished tremendously.